GLP1s increasingly not covered by insurance?

You'd think that GLP1 Receptor Agonist treatments, which help treat type 2 diabetes and help with weight management (and thus avoid some bad potential outcomes like Heart Disease or Diabetes) would be loved by insurance companies.
Check out our quick explainer
Turns out insurance companies are removing it from coverage at alarming rates, often due to cost.
Insurance providers that have removed Ozempic or other GLP1 drugs
We know that Ascension has dropped coverage of Ozempic and other (including future) GLP1 RAs for it's employees:

UT SELECT and UT Care prescription drug plans, administered by Express Scripts have dropped Wegovy and Saxenda for weight loss and weight loss management:
Plans that are covering GLP1 drugs (ex. Medicaid)
Right now, the biggest health plan that is guaranteed to be covering a drug like Ozempic is Medicare – but not for weight loss. Confused? We'll explain.
The University of Michigan has a great guide on this:

The important bit:
A law passed in 2003 prohibits Medicare from covering weight loss medications, though it can cover drugs to help people with Type 2 diabetes manage their weight.
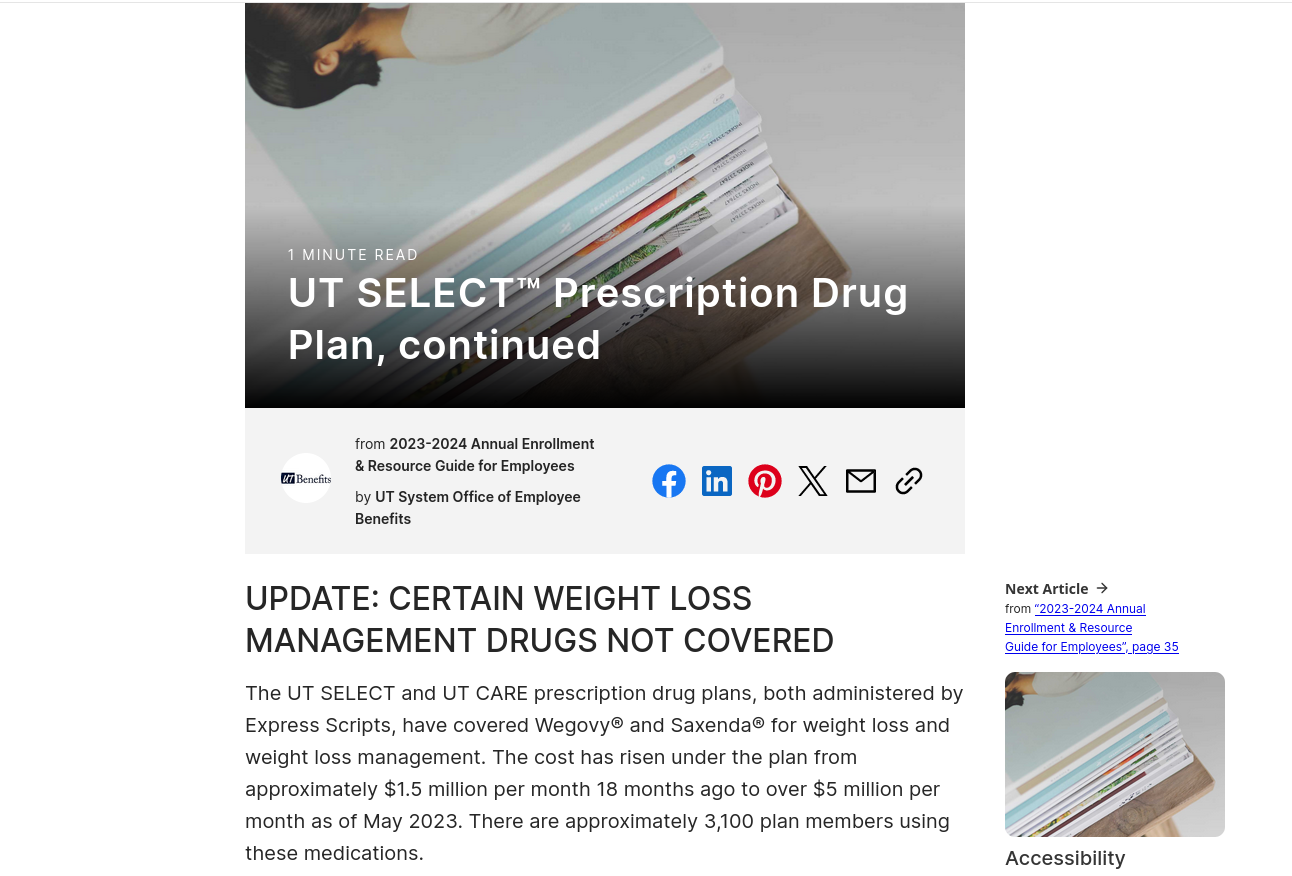
Medicaid covers obesity medications for adults with low incomes in 15 states. Most private plans and the Veterans Health Administration cover them, but with restrictions due to high monthly costs for the new generation of medications.
This means there's a difference between a drug like Ozempic which is FDA approved for treating type 2 diabetes, and Wegovy, which is approved for weight management/weight loss.
That said we know that Medicaid Part D (drug coverage) was actually modified to include GLP1 drugs.
That said, states are free to choose whether they cover the drugs or now, so there is some discrepancy – some states have states have committed, and others haven't:
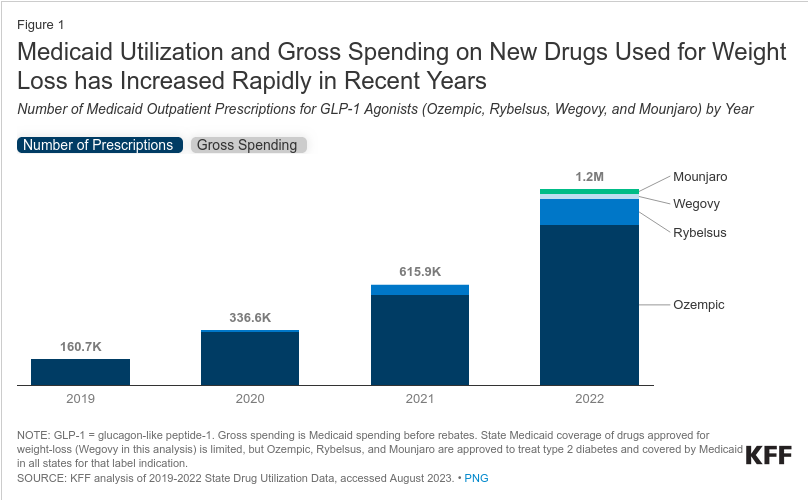
There are great sources out there cataloging the rise in prescription and use of GLP1 Receptor Agonists like Ozempic, Wegovy, Mounjaro, Rybelsus and others:
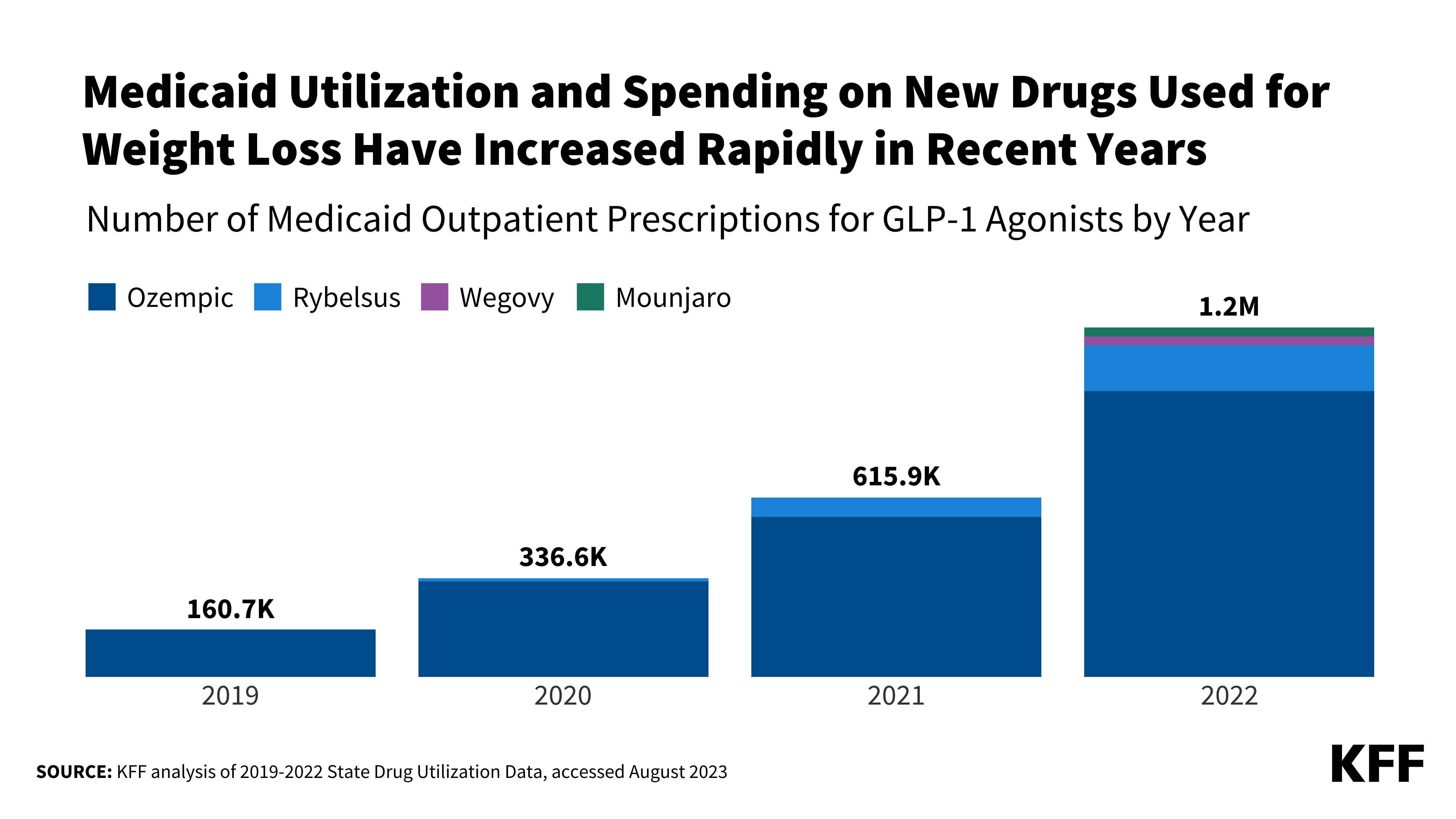
Looking at the chart that KFF produced:
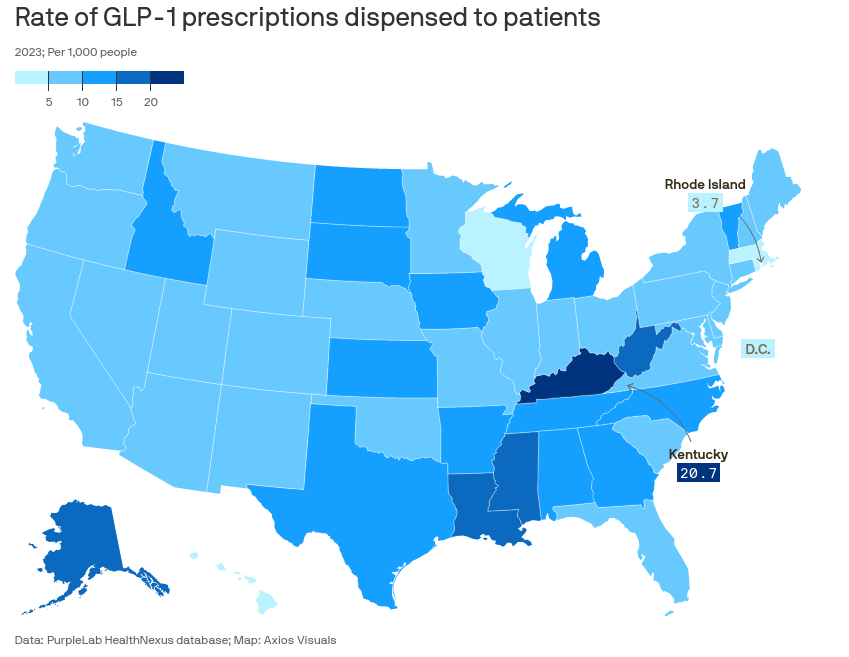
What this doesn't show is the actual rate of prescriptions, which is also huge, and put together by Axios:
So in the future, it's likely that more and more states will start to include the drugs in medicare, as more seniors and other citizens demand them.
So what? Cost is still the issue
Price and availability are still the key determining factors for whether GLP1 Receptor Agonists like Ozempic, Wegovy, Rybelsus and others can be added to health insurance plans and national options like Medicare.
Health plans like those at UT are unlikely to continue offering medication like Wegovy which are for weight management (rather than type 2 diabetes strictly), unless the prices are in line with what they can budget.
Even if on Medicare, since states are free to choose/manage which medications they support and offer under Part D, the importance of price is a major factor in the decisions of states to carry the drug or not, even with the federal rebate.